- Future Proof PT
- Posts
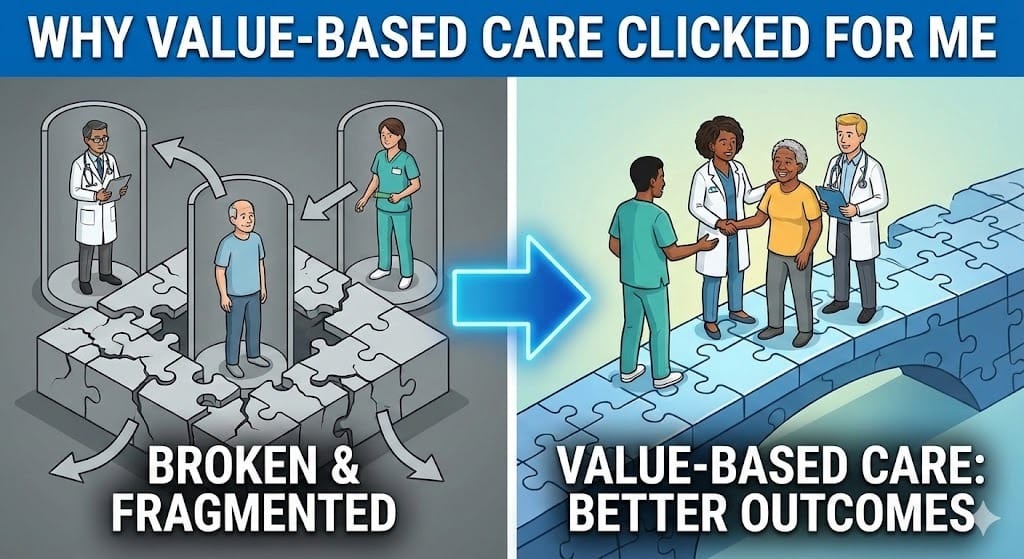
- Why Value-Based Care Clicked for Me
Why Value-Based Care Clicked for Me
From "failing therapy" to high-value outcomes. Why PTs need a seat at the table.
Subscribe to our sister newsletter below 👇️
|
Authored by Cody Lee, PT, DPT
Reason 1: We have a broken and fragmented healthcare system.
I have been a part of this system for going on 8 years now as a rehab tech, front office role and now physical therapist. I've seen care provided in the acute care setting and outpatient setting. I've witnessed how challenging it is to coordinate care between providers and the patient acting as the middle man. We live in silos focused only on what's in front of us, but when we zoom out there is a larger system at play. (For more on why we need to break out of professional silos, check out Dana Strauss' piece "Say No to Professional Silos!") I see value-based care (VBC) trying to incentivize that system to work better together and ultimately create better outcomes for the patient.
Reason 2: The largest healthcare payer in the U.S. is pushing the healthcare landscape towards VBC.
It would be foolish to not pay attention and act like this isn't happening. Rather than being reactive to the change, I want to be proactive. I don't want to be left behind trying to figure out how I fit within this system. Rather, I want to be a part of defining what it looks like for PT to fit in this system. If we continue as a profession to not have a seat at the table in these decisions we will be left behind.
Reason 3: I finally learned what decisions are being made, who is making them, and how I could potentially impact those decisions.
Healthcare policy drives everything we do as healthcare providers. The decisions we make on a daily basis are largely decided before we make them because of the policies that dictate how we operate. It makes sense to me that if I want a "say" then I need to understand the language of the people making these decisions, what matters to them and how I can play a role in shaping policy.
Why VBC and Healthcare Policy Keep Pulling Me Back
We have a fragmented healthcare system, the largest payer in the country is pushing towards VBC, and healthcare policy determines our roles as providers. Let me show you what this looks like in practice.
The Broken System in Action
In this fee-for-service world, the healthcare system is fragmented, broken and siloed. There’s often little collaboration between disciplines. The flow of information is disrupted or non-existent. Patients have to repeat themselves dozens of times and act as the true "middle man." There is no incentive within the current system to better coordinate care, decrease low value care, or collaborate.
This shows up in the narratives patients hear. Different providers tell them different things about their pain or condition. Sometimes these narratives hinder the next provider or hurt the patient directly.
A Patient Example
Let's think about a patient who is in their fifties and has been diagnosed with osteoarthritis (OA) of the knee. They are referred by their physician to be evaluated by a physical therapist.
I hear from patients like this in the clinic that they have been told they need to “go through therapy” or "fail therapy" before they can have an MRI or injection. If we think about this for a moment, how likely is it that physical therapy will be helpful for this patient now? 70%? 50%? 30%?
I'm going to say with a narrative like this, the likelihood of a patient having success with physical therapy is going to be less than 15%.
Put yourself in this hypothetical patient's shoes for a minute. If you were told that you needed to "fail" therapy before you can have the next step in the treatment plan, the step that you think is actually going to be helpful for you (either an MRI or procedure), you would probably put very little effort and stock into attempting physical therapy and complying with a treatment plan.
Now, let's flip the scenario.
This time, the patient is told by the physician "We hear that you are experiencing pain in your knee, and from the x-ray, we can see that you have some knee osteoarthritis. Osteoarthritis is a degenerative joint condition that becomes more common with age. The good news is that conservative management and lifestyle modifications, such as exercise, weight management, and improving sleep quality, have a good chance of improving your symptoms and function. Research shows that strengthening the muscles around your knee can reduce pain and help you stay active. Surgery is not the first line of treatment in your case--conservative management is the treatment path I would recommend and it should at least delay and perhaps allow you to avoid surgery.”
One narrative is fairly negative, one fairly positive. The outlook for the patient hearing these narratives will be quite different. (Research published in JOSPT shows how "impairment-based" language like "fail therapy" discourages engagement, while "participatory-based" language empowers patients to take an active role in their care.) I would argue that the buy-in for this patient is going to dramatically change and the probability of success would shift to perhaps greater than 60%.
Why Does the First Narrative Exist?
The question then is "Why would the second narrative not be given in the current system?"
It goes back to financial incentives in the structure of fee-for-service reimbursement. The healthcare provider is incentivized to provide more services because more services equals more money, and the system does not reimburse for the extra 10 minutes it takes to have the more comprehensive conversation. That conversation also puts the patient first, and respects their crucial role in the healthcare team.
Unfortunately, the patient's outcome (cost and quality) is not what pays the physician's bills.
If the physician and patient have the second conversation, it would increase the odds of success with conservative management. If the patient improves with PT and does not require an image or procedure then the referring provider doesn't get to increase their volume. Where the "fail therapy" narrative is not likely given intentionally to sabotage PT, the current system does subconsciously incentivize that.
We are all a function of the system we operate within. This is a great example of that.
To think further on that, the provider likely faces pressure from administration, overhead, increasing expenditures and decreasing reimbursement. So it makes sense that they would do what they can to increase volume.
This is where VBC offers something different. It's a system change that incentivizes the right things. What is best for the patient, provider, and payer.
Show me the incentives and I’ll show you the outcome.
What VBC Changes
Imagine that same physician is in a VBC arrangement where reimbursement is tied to reducing low value care and increasing the successful use of lower cost treatment alternatives. Now they're incentivized to help this patient see the value in physical therapy and successfully avoid or postpone higher cost interventions to manage their knee OA.
The patient would be seen by the right provider, at the right time, and receive the right care when they go see their physical therapist. This time, their physician's nudge was different. They implied "physical therapy and some lifestyle adjustments are the right approach to manage your OA right now."
The Shift is Happening
CMS has set a goal for all Medicare beneficiaries to be in a VBC arrangement by 2030. If that's where the system is heading, wouldn't it be foolish to not learn more about it?
I have found that our profession is often reactive to what is happening around us rather than proactive. We tend to complain from the sidelines rather than raising our standard and joining the conversation directly. We need to engage with CMS and the Center for Medicare and Medicaid Innovation (CMMI) in order to have a seat at the table.
As for me as an individual clinician, I want to be a part of the solution that helps define what it looks like for PT to fit within the VBC system. I hope I'm not alone. As Dana Strauss puts it, "If you are a physical therapist (or OT or SLP), you have never been more valuable than you are right now. Demonstrate that value to at-risk providers."
Consider this: a MedPAC report (page 85) identified sources of low value care. There are several billion dollars worth of low value care specifically in the MSK domain that PT can directly impact with high value care.
Now, we can have a debate on whether PT is inherently high value or what distinguishes high value from low value PT another time. But briefly, high value PT includes quality patient education, considering the whole person, progressive therapeutic exercise, and increasing a patient's self-efficacy to manage their symptoms and improve function. Low value PT looks like only treating symptoms with band-aids (think passive modalities), creating a dependency where the patient "needs" you, and using nocebo language that reinforces fear and avoidance. The nuance deserves its own conversation.
The point is, there are opportunities for PT to have a direct impact in the VBC system. But if we are not paying attention, don't understand what matters to CMS, or remain in denial, we will never have a seat at the biggest tables.
Policy Drives The Business of Healthcare Delivery
Once I began to understand where decisions are being made, how those decisions affect us, and who is making them, I became drawn to healthcare policy.
News flash: PTs are not influencing the policy changes that determine how we practice and are reimbursed for the care we provide.
CMS establishes the foundation for how healthcare providers get paid. According to Milliman's commercial reimbursement benchmarking data, many commercial fee schedules utilize Medicare-like reimbursement structures, making Medicare rates the reference point for the entire system.
In large part, how we are paid and the amount our codes are worth are decided by the Relative Value Scale Update Committee (RUC) from the American Medical Association. This committee is largely made up of physician specialists with one rotating allied health provider. The codes we bill are not determined by PTs.
The worth of your knowledge and expertise is being determined by someone else.
But whose fault is that? It's easy to point the finger and blame others, but what have we done as a profession to become more involved in influencing the policymakers who hold the pen in allocating funding among and between clinician types?
Healthcare policy drives the decisions we make as providers on a day to day basis. Our workflow and patient management are a product of the reimbursement structures created by policymakers and related committees. Where do supervision requirements come from? Where do time requirements for billing come from? Why can't we get paid for higher complexity evals compared to lower complexity evals? Why do practice acts vary from state to state?
Because of healthcare policy.
It begins and ends with policy.
The Choice
So if that's the case, I want to learn everything I can about healthcare policy. The language these folks speak, what they care about. So that I can begin to help shape it.
That's why VBC and healthcare policy keep pulling me back.
You can do three things in any situation: accept it, change it, or leave it.
I choose change.
|
